Nearly 50 percent of people worldwide are deficient in Vitamin D. This number is higher amongst those of us who live in more northern climates. Vitamin D, or the sunshine vitamin, is actually a steroid hormone that our bodies make in response to ultraviolet light (UVB specifically).
The UVB rays from sunlight trigger the production of Vitamin D3 (cholecalciferol) in our skin. This compound must then go through additional steps in both the liver and kidneys to become the active form of vitamin D3, which is calcitriol. Being able to manufacture our own vitamin D seems like a pretty nifty trick right? Why then are nearly 50 percent of us deficient in vitamin D?
First, a little history lesson. Way back in the early 1600’s, the world was undergoing an industrial revolution. People were beginning to live in large cities, with housing being built close together and pollution from coal burning creating a haze in the air. It was around this time that a disease called Rickets began appearing in children. Rickets is a bone deforming disease that we now know is caused by a Vitamin D deficiency. The connection between the lack of sun exposure and Rickets was probably first made in the 1800’s by Polish physician Jedrzej Sniadecki.(1) He noticed that children in populated areas such as Warsaw, receiving little sunlight due to narrow alleyways, pollution and tight living quarters, had a higher incidence of rickets that those living in rural areas outside of Warsaw. In response to this observation, Sniadecki recommended in his book, On the Physical Education of Children (1822), that children “should be carried about in the open air especially in the sun, the direct action of which on our bodies must be regarded as one of the most efficient methods for the prevention and the cure of this disease.”(2)
Although most of Vitamin D’s fame comes from it’s role in aiding in the absorption of calcium and creating healthy bones, it is actually involved in a large number of important functions in our bodies. It plays a role in both immune function and control of inflammation. Therefore, it may be crucial in the management of both autoimmune and inflammatory diseases. It helps to regulate the release of a neurotransmitter called serotonin, which is important for both mental health and digestion. It is essential for healing, as it helps control cell growth. Vitamin D’s control over cell proliferation, along with its anti-inflammatory effects may have protective effects against many cancers. Scientists continue to study Vitamin D and its benefits to our health. The role of Vitamin D deficiency in heart disease, mental health, obesity and Parkinson’s disease are just a few of the many areas being studied.
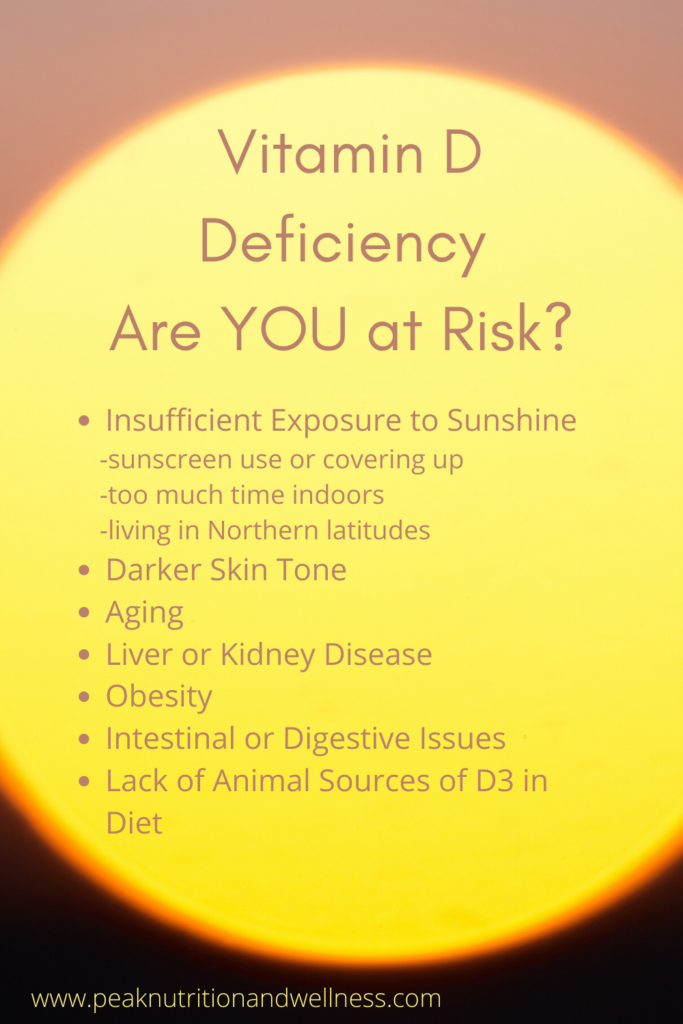
So back to the original question – why are over 50 percent of us deficient in this important nutrient? The obvious answer is that we are not getting enough sunshine! There is a reason it is called the “Sunshine Vitamin”! Along with living at a higher latitude, our jobs and hobbies (I’m looking at you Netflix) are keeping us out of the sunshine. When we do venture out, we slather on the sunscreen, afraid of skin cancer and (yikes!) wrinkles. It is also difficult to get anywhere near enough Vitamin D from the food we eat. It can be found in the oil of fish livers (think cod liver oil) and there is a small amount in egg yolks and fatty fish, like salmon, sardines and mackerel. Plant foods, like mushrooms and leafy greens, contain a very small amount of Vitamin D2. It is thought, however, that this plant derived from of vitamin D doesn’t seem to perform all the functions that animal derived D3 does. Many foods, such as homogenized milk and breakfasts cereals are fortified with Vitamin D. Even if you aren’t avoiding these processed and packaged foods, in order to get your daily requirement of Vitamin D, you would have to consume an unfeasible amount of these foods!
So Who is at risk?
- Digestive Issues – Even if we could consume enough vitamin D in our diets, we are assuming that it is all going to be absorbed. The health of your gut is going to influence how much of the vitamin you absorb and, let’s face it, many of us have at least some digestive issues. Issues like celiac disease, Crohn’s disease, disorders (or absence) of the gallbladder can all reduce vitamin D absorption. These efficacy of vitamin D supplements are also affected by these digestive issues.
- Obesity – Vitamin D is a fat soluble vitamin and is stored in fat tissue. Obesity means we have more fat in which to store that Vitamin D, making it less easily accessible when needed.
- Darker skin tones – Higher amounts of the pigment melanin in dark skin tones acts as a natural sunscreen, reducing the amount of Vitamin D produced
- Increased Age – Lower amounts of the precursor to Vitamin D, skin changes and more time spent indoors increases the risk of deficiency in older individuals
- Time of year and location – UVB rays are weaker in the northern latitudes, so weak in fact that there are large periods of the year (4 to 6 months) when one just can’t make enough Vitamin D from sun exposure alone. (3)
How do I know if I’m deficient?
The symptoms of Vitamin D deficiency are often so subtle that you have no idea you are deficient. I know that I had no clue, until my blood test came back! The effects of vitamin D deficiency are varied and we rarely make the connection between these signals and a lack of vitamin D. They may include:
- Fatigue
- Bone pain
- Muscle or Joint pain
- Frequent Illness
- Low mood or irritability
- Anxiety
So what can you do?
Advocate
Ask your physician for a blood test. Vitamin D levels are not something that most physicians will order with your yearly bloodwork. Because there are no overt signs of deficiency, I think it is important to know what you level is – especially if you fall into one of the groups who are more at risk for a deficiency.
Conventional “normal” ranges can vary depending on the lab conducting the test. They are also based on the average population which, if we are being honest, is not all that healthy. Generally, the “normal” range will be quite wide (30ng/ml to 100ng/ml). But this normal range doesn’t necessarily reflect what is healthy, only what is common. Functional references ranges are narrower and reflect a level that is optimal to prevent dysfunction and, eventually, disease. A functional optimal range for vitamin D is much narrower, perhaps at 60ng/ml to 80ng/ml. When disease is present, such as with heart disease or cancer, the optimal range may be higher.
Supplement
Most of us living in northern latitudes are not going to be able to get all the vitamin D we need year round. A high quality supplement can help us keep our levels up throughout the year.
The amount of vitamin D to supplement will vary depending on your current blood level, health status and sun exposure. As always, it is important to have a discussion with your health care provider to determine an appropriate dose and have your levels monitored periodically. Also, always…ALWAYS consult your doctor or pharmacist before starting any supplementation, in order to rule out drug interactions or contraindications!
As vitamin D is fat soluble, there is a risk (although extremely small) of toxicity, because excess can be stored in the body. It is generally only seen in those who take extremely high doses for long periods of time.
Sunlight
Overall, sun exposure really is the best source of vitamin D, as we don’t have to rely on adequate digestion for it to reach our bloodstream and get to work! It is a bit of a balancing act, especially if you are like me and go from bright white to lobster red in the blink of an eye. A general rule of thumb is for the time of sun exposure to be 50% of what it would take to cause a mild sunburn (slight pinkness 24 hours later). After this time, slather on the safe sunscreen, cover up or seek shade.(1) For me, that’s probably about 5 minutes in the mid-day summer sun! The more skin that is exposed, the more vitamin D those factories in your skin will produce. I would recommend protecting the face with sunscreen or a hat, as it’s surface area is relatively small and will produce only a small amount of vitamin D and the skin there is more prone to damage from sun exposure.
The other benefit of getting Vitamin D from the sun? Toxicity is not an issue. There are compounds made along with the Vitamin D that will limit any excess production, protecting us from toxicity. The body is a wondrous thing, isn’t it?
References
- Wacker, M., & Holick, M. F. (2013). Sunlight and Vitamin D: A global perspective for health. Dermato-endocrinology, 5(1), 51–108. https://doi.org/10.4161/derm.24494
- Mozołowski W. Jędrzej Sniadecki (1768-1838) on the Cure of Rickets. Nature. 1939;143:121. doi: 10.1038/143121a0
- https://academic.oup.com/ajcn/article/79/3/362/4690120(Holick MF. Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004; 79:362-71)