I’ve been lucky, I think I’ve only ever experienced heartburn once in my life. It woke me from a deep sleep and had me frantically digging through my kitchen cupboards at 3am, looking for some sort of relief. We aren’t milk drinkers, so I couldn’t try that old remedy. I had a surprisingly empty medicine cabinet for a pharmacist, only some first aid cream and bandages. No Tums, no Gaviscon, no aBISMALly pink Pepto-Bismal. I decided to use my half awake, “sciency” brain and tackle the acid with its known nemesis – a base. Baking soda to the rescue. I mixed it with some water and took it like a shot. It was, well, it was awful. Not something I’d want to have to do regularly. It took a little time, but the fire finally subsided enough for me to crawl back into bed, bedside my blissfully unaware husband, praying that the inferno wouldn’t return.
For many people, the discomfort of heartburn, indigestion or reflux is a daily occurrence. Just walk through the stomach section of any pharmacy and you’ll see just how prevalent these issues are. In my years in the pharmacy, prescriptions for acid reflux medications flew off the shelves. It was an equal opportunity Rx too! Men, women, young and old. Everyone needed their “stomach pills”. But just because these tummy troubles are common, does not mean they are normal. Instead, they are a sign that there is something amiss and your body is letting you know that all is NOT normal.
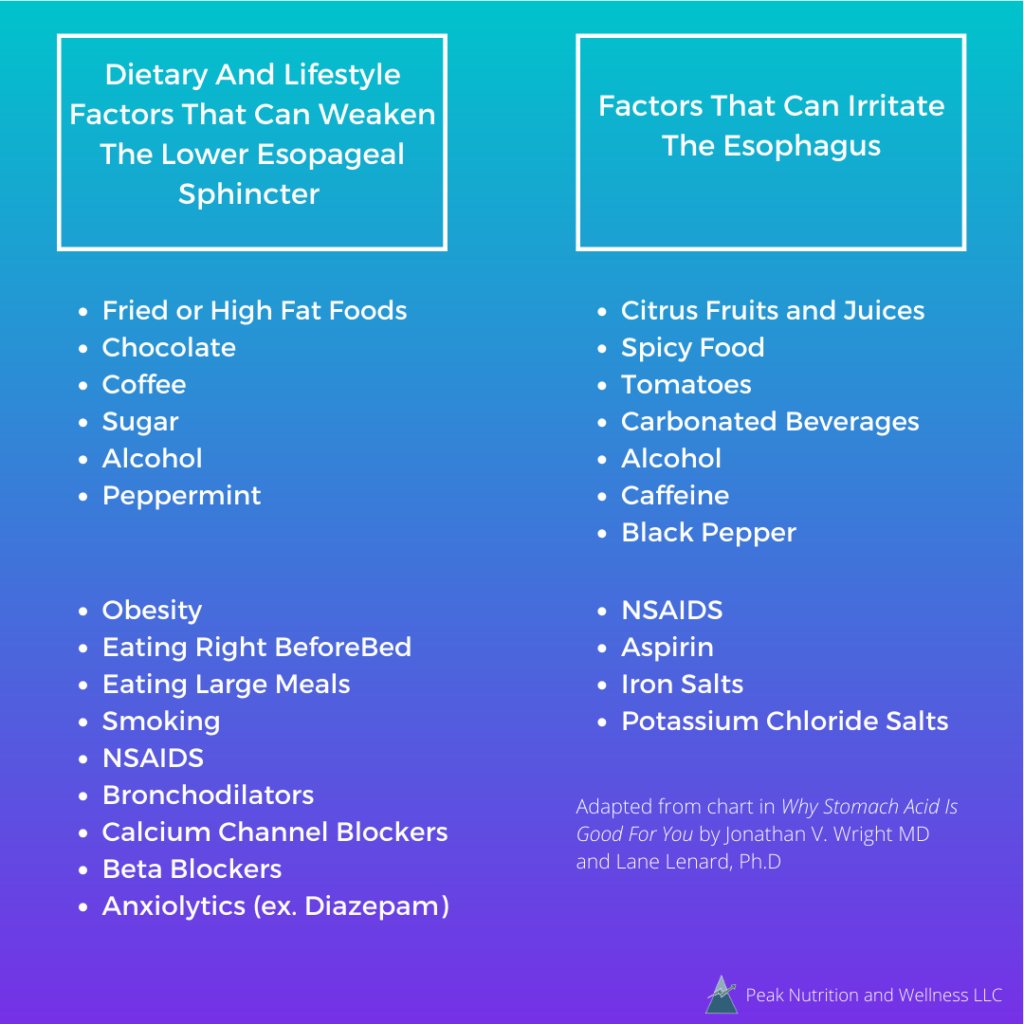
Why are there so many “fire breathers” around these days? Why do so many people produce such vast quantities of stomach acid that they need to be on a medication to control it? The truth is, they don’t. Over-production of stomach acid is a very rare condition (Zollinger-Ellison Syndrome) and it only affects about 1 in 1 million people. There can be a couple of factors at play here. One is that certain dietary and lifestyle habits can relax the Lower Esophageal Sphincter (LES). The LES is the gateway between the esophagus and the stomach and it is meant to stay tightly closed to prevent stomach acid from coming into contact with the unprotected tissue of the esophagus. When you only experience symptoms once in awhile, simply changing some habits and avoiding those foods that trigger your symptoms will often suffice.
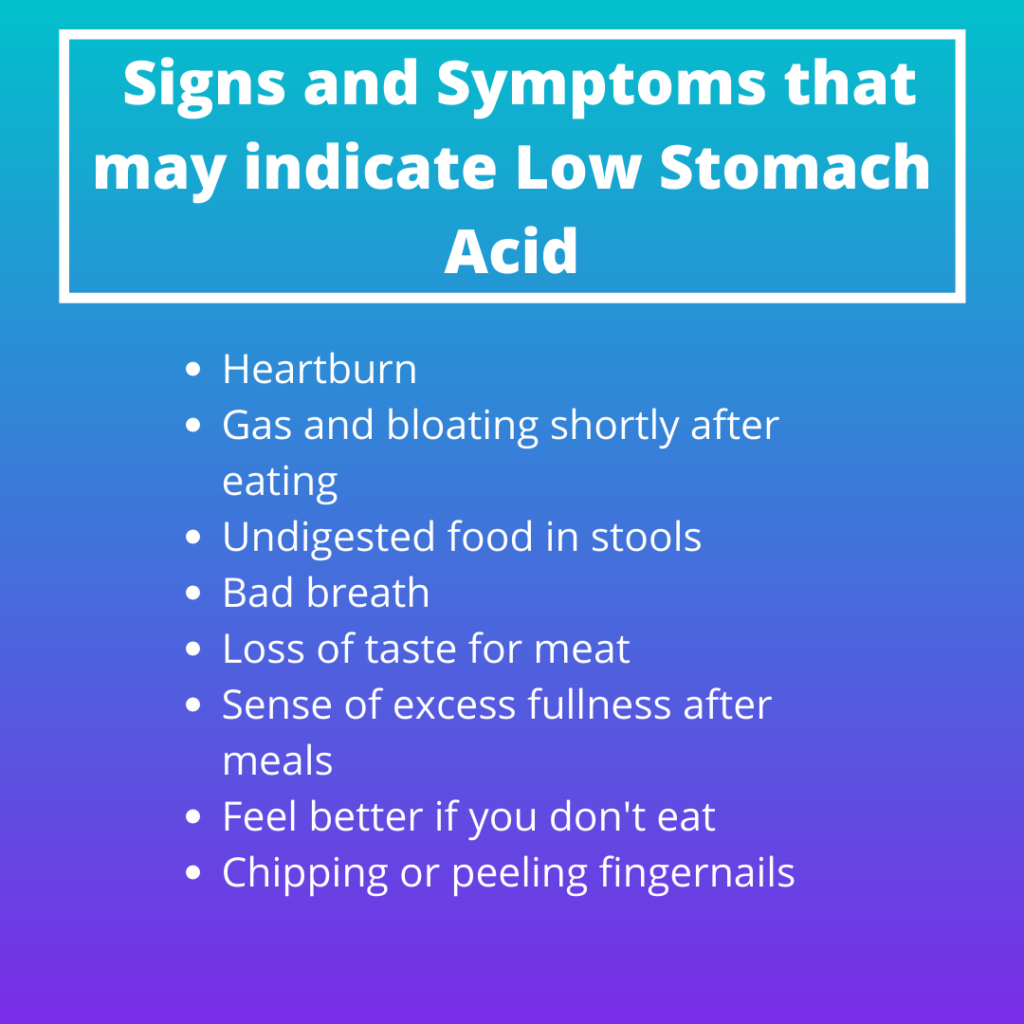
The most common cause though, the ROOT cause, of these symptoms is actually insufficient stomach acid. Yes, wrap your brain around that. The current recommended remedies for heartburn and indigestion not only fail to treat the cause of the symptoms, but contribute to them and many more problems. This is the concept behind the book Why Stomach Acid Is Good For You by Johnathan V. Wright M.D. and Lane Lenard Ph.D.
Wright and Lane propose that it is a lack of stomach acid that causes heartburn, indigestion and GERD and to properly treat the cause, the acid must be replaced. Drugs prescribed for these conditions turn off production and decrease stomach acid even further. They appear to help because they cover up the symptoms (your body’s way of messaging you that something is wrong), but they are actually potentiating the problem. So why is low stomach acid a bad thing, if it makes us feels so much better?
Stomach acid plays a vital role in digestion. One of the key components of the gastric juices is HCl (hydrochloric acid). HCl is necessary to break proteins down into amino acids, which can then be absorbed. Many other nutrients require an acidic environment for absorption as well. Stomach acid is also the starter pistol or trigger for almost every other event in the digestive sequence. Without stomach acid, digestion functions about as well as car on empty.
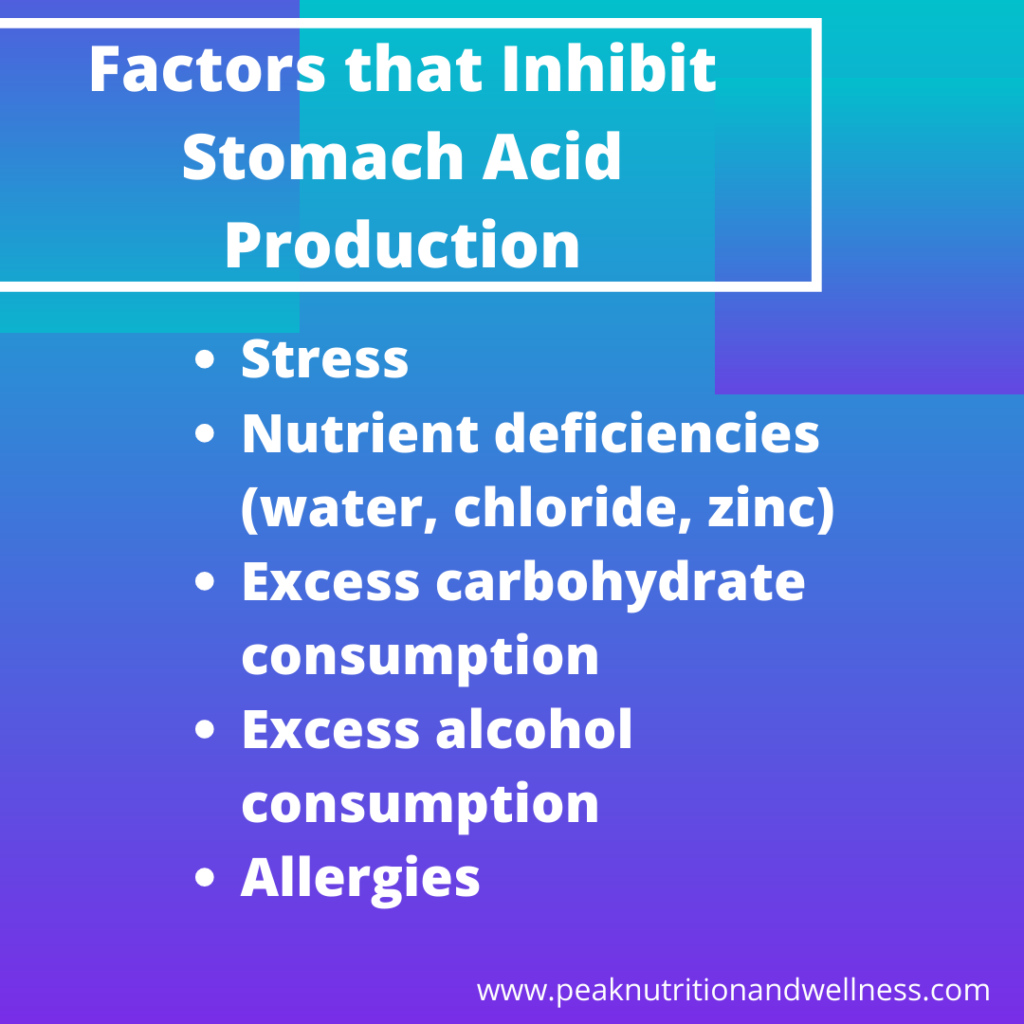
The acidity of the gastric juices makes the stomach a sterile environment. Stomach acid kills pathogens that we ingest with our food. As well as protecting us from infection, this acidic environment prevents bacteria from surviving in the stomach and interfering with the digestion of certain nutrients. The negative consequences of low stomach acid continue to affect our digestion all the way down the line. I discuss the consequences (ad nauseam) in THIS blog post, if you want to get into the nitty gritty!
I found it interesting to learn that the cells that produce HCl (parietal cells) decrease as we age. Much of the malnutrition we see in senior citizens maybe caused by low stomach acid and treatable with acid supplementation. The authors discuss how nutrient deficiencies caused by low stomach acid may contribute to several conditions from depression all the way to rosacea. Besides nutrient deficiences, the book also looks at how low stomach acid leads to large, undigested protein molecules. These can make their way through the lining of the small intestine (made “leaky” by the damage of bacteria growing in the low acidic environment of the stomach). These large food molecules enter the bloodstream. They are not broken down enough to be recognized by the immune system, are tagged as foreign and attacked. Overtime, this immune system activation can cause food sensitivities and contribute to the development of autoimmune conditions.
Although I did find the authors somewhat wordy and repetitive, there was a lot of good information in this book. The link between low stomach acid and the myriad of problems it may contribute to makes common sense, even if there are few quality studies to support some of these claims. (I mean, a drug company is not likely to fund a study that may show their product is unnecessary at best and harmful at worst!) As it was published in 2001, it would be nice if there were a newer edition of the book to highlight any current information in this area. I don’t know that I can agree wholeheartedly with some of the authors’ ideas that low stomach acid may be the out right cause of certain diseases. I certainly can agree that it could be a contributing factor and, as such, it is prudent to optimize stomach acid and digestion in all conditions.
Please note, that if you are currently on a medication that lowers stomach acid, I am NOT recommending that you stop this treatment. Seek out a Functional Nutritional Therapy Practitioner (like moi), who can help you make some dietary and lifestyle changes that support digestion. Once those are in place, you can talk to your physician (or ideally your FNTP and physician can work together!) to discuss whether you need the medication, create a plan to wean off the medication and possibly start some acid supplementation, if needed, all while monitoring your symptoms.