
Chances are, if you’ve done any reading on health in the last decade, you’ve seen the term microbiome. But what exactly is it? Why are scientists and health professionals so enamoured by it? And why the heck should you care?
Your ‘Gut Garden’ aka Microbiome
Your microbiome is the community of micro-organisms that live in and on your body – in your mouth and nose, on your skin and the surface of your eyes and in your gastro-intestinal tract. There are trillions, yes, TRILLIONS of bacteria, fungi, viruses and even parasites co-existing with us everyday.
I like to think of the gut as a garden, with the bacteria that support our health being the flowers and the non-beneficial, or potentially detrimental, microbes being the weeds. Like any garden we want to feed and nurture the flowers, while keeping the weeds under control.
If the thought of bajillions of microbes existing in and on you gives you the heebie-jeebies, fear not. We NEED these little guys for so many things and, as long as everything is in balance (plenty of flowers and not too many weeds), it’s a mutually beneficial relationship.
Roles of the Microbiome
The microbiome, particularly the gut microbiome, is a hot topic for health research these days. Researchers have made many connections between a person’s overall health and the health of their gut garden and the consensus is that there are still many more discoveries to be made.
Our microbiome is an integral part of almost every single aspect of our health. Some of the roles it plays include:
- Supports the immune system by keeping “bad” bacteria/pathogens in check (1)
- Helps us digest and extract nutrients and energy from food (1)
- Produces chemicals that improve the health of the cells of our intestinal lining (1) (2)
- Produces vitamins, such as Vitamin K, thiamine, folate, biotin, riboflavin and pantothenic acid (3)
- Acts as our second brain and affects our moods and motivation by producing chemicals that positively influence brain health, including serotonin and dopamine (4)
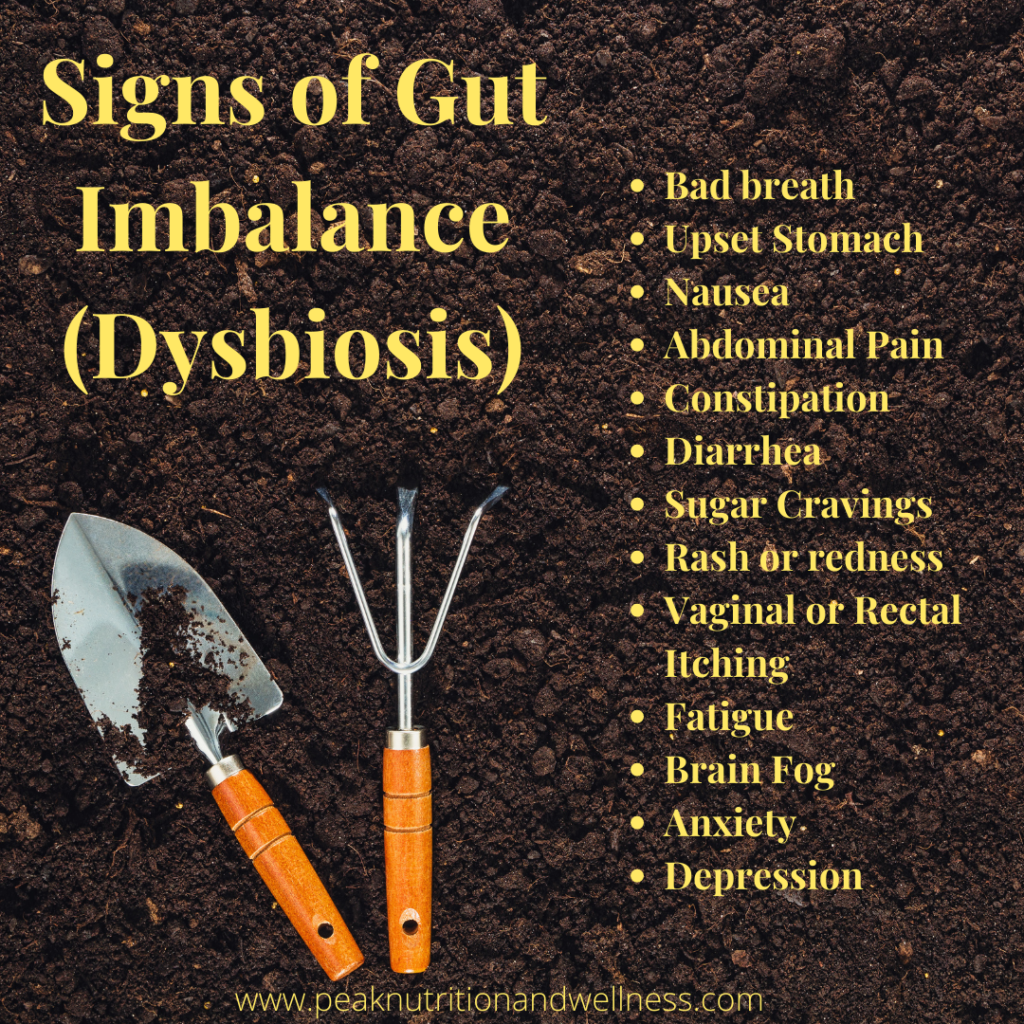
Signs that all may not be well in your garden
When we don’t have enough beneficial bacteria and/or have too many non beneficial microbes in our gut, it’s called dysbiosis. The signs and symptoms of an imbalanced gut, or dysbiosis, are wide ranging and, as you’ll see, there are many you would not automatically associate with the health of your gut garden.
What impacts the health of your gut garden?
So. Many. Things.
Frequent rounds of antibiotics growing up, dietary choices, not being breastfed as an infant, not properly breaking down our food, stress, chemicals and toxins in our food and personal care products….the list is long!
The good news is that, while there are some factors we have no control over, there are plenty of things we can do to nurture and support the health of our microbiome. Your gut garden is constantly changing depending on your environment, lifestyle and what you feed it.
How to tend to your garden
Just as there are many things that negatively impact the health of our microbiome, there are also lots of things we can do to support those health promoting microbes.
Eat Your Veggies/Feed the Good Guys – Vegetables are loaded with fibre. Us mere humans can’t digest these fibres, but the good bacteria in our guts love it! They consume these fibres and produce short chain fatty acids which, among other things, help build and maintain a strong gut lining. Getting a wide variety of fibre-ific veggies on your plate can also help bolster the diversity of your microbiome (more types of flowers growing in your garden).
Exercise – Physically active people have more robust and diverse microbiomes. This may be due in part to exercise’s ability to help us burn off some stress.
De-stress – Stress is a double edged sword when it comes to your gut health. Too much stress can negatively impact your microbiome and an unhealthy microbiome can impair your ability to manage stress and your mental health. Put self-care on your “To-Do’ list by incorporating more “me” time, whether that’s meditation, time in nature, exercising or just saying no to things more often.
Eat Fermented Foods – Naturally fermented foods are a great source of probiotics. The bacteria and yeast that cause the fermentation and make these foods so yummy also boost the population of the beneficial microbes in your gut. This means more flowers to crowd out the weeds! Sauerkraut, kimchi, kombucha and kefir are good sources. Just make sure they are raw and not pasteurized. The heat involved in pasteurization will kill the good microbes.
Don’t Overdo Antibiotics – Sometimes antibiotics are necessary but, as their name suggests, they kill bacteria, regardless of if it is beneficial or non-beneficial. Avoid antibiotics in hand sanitizers and other personal care products. Ensure the meat you buy is antibiotic-free. If you do find yourself in a situation where you need an antibiotic, work with a Nutritional Therapy Practitioner to both support your microbiome during and rebuild it after your course of antibiotics.
Cut out Sugar and Processed Foods – Not only do these foods contribute to inflammation in the intestines, they provide no usable food for our good bacteria and we want to feed these good guys!
Get Your Zzzz’s – Aim for 7-8 hours of sleep a night. Growing evidence is showing that not getting enough shut-eye may disrupt the microbiome (5) and increase your chances of developing inflammatory diseases. Good sleep hygiene, like avoiding screens 1 – 2 hours before bed, ensuring your room is dark, cool and quiet and not eating right before bed, can go a long way in ensuring you get your 40 winks.
Test Don’t Guess! – We can do a lot of things to support our microbiome, but to find out what’s actually going on in there, you need to test. Symptoms can suggest there is a gut imbalance, but testing is the only real way to know if there is an infection, not enough good guys to keep the bad guys in check or issues with properly breaking down our food. I use two tests in my practice, the GI Map stool test and the MRT food sensitivity test. Used together, we can determine what is contributing to the issues in the gut, lower the inflammation driving the symptoms, heal and seal that gut lining and restore the balance in your gut garden.
I’ll be talking more about these tests in future posts. Until then, if you are thinking your gut garden might be in need of some tending, reach out! I’d love to chat and explore your options for restoring balance and healing that gut!
Sources
- Zhang, Y.J., Li, S., Gan, R., Zhou, T., Xu, D.p., & Li, H.B. (2015). Impacts of gut bacteria on human health and diseases. International Journal of Molecular Sciences, 16(4(, 7493-7519. https://doi.org/10.3390/ijms1607493
- Flint, H., Scott, K., Louis, P. et al. The role of the gut microbiota in nutrition and health. Nat Rev Gastroenterol Hepatol 9, 577–589 (2012). https://doi.org/10.1038/nrgastro.2012.156
- Morowitz, M. J., Carlisle, E. M., & Already, J.c. (2011). Contributions of intestinal bacteria to nutrition and metabolism in the critically ill. The Surgical Clinics of North America, 91(4), 771-vii. https://doi.org/10.1016/j.suc.2011.05.001
- M Hasan Mohajeri, Giorgio La Fata, Robert E Steinert, Peter Weber, Relationship between the gut microbiome and brain function, Nutrition Reviews, Volume 76, Issue 7, July 2018, Pages 481–496, https://doi.org/10.1093/nutrit/nuy009
- Smith, R. P., Easson, C., Lyle. S. M., Kapoor, R., Donnelly, C. P., Davidson, E.J., Parikh, E., Lopez, J.V., & Tartar, J.L. (2019). Gut microbiome diversity is associated with sleep physiology in humans. PIoS one, 14(10), e0222394. https://doi.org/10.1371/journal.pone.0222394

